Transient loss of consciousness after Thoracic Endovascular Aortic Repair (TEVAR).
Key points in the management of such cases.
Key points in the management of such cases.
| Available Online: | Desember, 2022 |
| Page: | 96-99 |
Author for correspondence:
Schizas Nikolaos, MD , MsC , Phd(c)
National and Kapodistrian University, Athens, Greece Rimini 1, 15772
Tel: +30 6936820715
E-mail: nikschizas@gmail.com
Schizas Nikolaos1, Nazou Georgia2, Patris Vasilios1 , Lama Niki3, Toulgaridis Fotios4, Kratimenos Theodoros5, Argiriou Mihalis1
1 Department of Cardio Thoracic and Vascular Surgery, Evangelismos General Hospital of Athens, Athens, Greece
2 Anesthesiology Department, Evangelismos General Hospital of Athens, Athens, Greece
3 Research Unit of Radiology and Medical Imaging, Kapodistrian University of Athens, Greece
4 Cardiology Department, Evaggelismos General Hospital of Athens, Greece
5 Department of Radiology, Interventional Radiology Unit, Evangelismos General Hospital of Athens, Athens, Greece
Abstract
Full Text
References
Images
Abstract
Thoracic Endovascular Aortic Repair (TEVAR) is the main invasive option in the management of type B aortic dissection, but there are still some points in the application of such techniques that are controversial. In this article, we present a case report of a 71-year-old man who was admitted for a TEVAR procedure for a type B Stanford dissection. Transient loss of consciousness occurred the second day after TEVAR and subclavian steal syndrome (SSS) was diagnosed, which was treated by a carotid-subclavian bypass. On the occasion of this case, some aspects about the preoperative assessment, the necessity and indications of left subclavian artery revascularization before TEVAR are presented.
Keywords: Thoracic Endovascular Aortic Repair, Subclavian steal syndrome, Left subclavian coverage, syncope, vertebrobasilar
Full Text
INTRODUCTION
Thoracic Endovascular Aortic Repair (TEVAR) is evolving rapidly as more and more knowledge is added, although there are still some parameters that need to be delineated. Occlusion of the left subclavian artery (LSA) is often necessary in order to ensure an adequate proximal landing zone1,2. Coverage of the left subclavian artery by stent-graft is associated with a not negligible incidence of malperfusion, including signs of claudication and ischemia of the arm or subclavian steal syndrome (SSS), which may be present in 9,5% of patients.3 SSS is usually presented with paresthesia of the left arm during exercise, symptoms of vertigo or dizziness, episodes of syncope while an elevated difference in the measurement of arterial pressure is detected between both arms.4
In this article, the case of a 71-year old man with transient loss of consciousness associated with specific movements after TEVAR is presented.
CASE REPORT
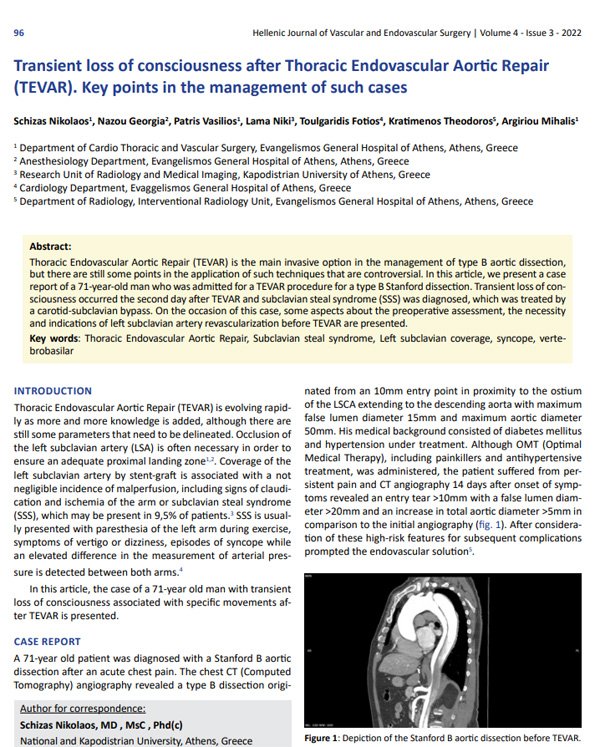
A 71-year old patient was diagnosed with a Stanford B aortic dissection after an acute chest pain. The chest CT (Computed Tomography) angiography revealed a type B dissection originated from an 10mm entry point in proximity to the ostium of the LSCA extending to the descending aorta with maximum false lumen diameter 15mm and maximum aortic diameter 50mm. His medical background consisted of diabetes mellitus and hypertension under treatment. Although OMT (Optimal Medical Therapy), including painkillers and antihypertensive treatment, was administered, the patient suffered from persistent pain and CT angiography 14 days after onset of symptoms revealed an entry tear >10mm with a false lumen diameter >20mm and an increase in total aortic diameter >5mm in comparison to the initial angiography (fig. 1). After consideration of these high-risk features for subsequent complications prompted the endovascular solution5.
The coverage of the left subclavian artery was necessary in order to ensure a safe proximal landing zone for the stentgraft placement. An endovascular occlusion of the prevertebral subclavian artery was performed with a Vascular plug in order to prevent type II endoleak (CELA, Vascular plug system).
Two endografts were placed consecutively with dimensions for the proximal 46 x 38 x 200mm and for the distal 42 x 38 x160mm (LifeTech endograft). The operation was performed under local anesthesia and sedation with maintenance of stablehemodynamics (heart rate 70-90/minute and Mean Ar- terial Pressure around 80mmHg). Intravenous morphine and paracetamol were administered for analgesia. The procedure was completed uneventfully.
The second day after the TEVAR, the patient suffered from an episode of transient loss of consciousness during mobilization. Careful clinical examination of the patient revealed that he presented loss of consciousness after lifting his left arm and also when he turned completely his head to the left. In addition to this, the situation was deteriorating as syncope occurred more often and with softer movements than the time of initial presence. Subsequently, a triplex ultrasound test was performed which detected the presence of SSS with a retrograde left vertebral flow. The CT scan examination from the vertex to the upper abdomen revealed an hypoplastic right vertebral artery.
A carotid-subclavian bypass with the use of 8mm Dacron prosthetic conduit (Vascutek Inc) was performed the next day. After the carotid subclavian by pass, there were no incidence of syncope regardless of the body movement or position. A CT angiography of neck-chest-abdomen was performed the 3rd day after TEVAR and the second after carotid- ubclavian bypass which showed a well positioned and functional carotid-subclavian bypass (fig. 2).
The patient was discharged the 4th post-operative day in good clinical condition. According to the follow-up protocol, he was submitted to repetitive CT angiographies in 1 month and 6 months for the intervention which were satisfactory enough with significant reduction of the false lumen and remodeling of the descending aorta. (fig. 3)
DISCUSSION
This case report reveals some points that are crucial for the management of patients submitted to TEVAR. Firstly, in the presence of acute or subacute aortic dissection type B with complications, malperfusion, resistant pain and hypertension in combination with feasibility of endovascular repair, TEVAR is indicated with Class I recommendation based on the guidelines of the European Society of Vascular Surgery, although the level of evidence is still low6 . Secondly, the size and the type of endograft is chosen after meticulous evaluation of the characteristics of the aorta, such as diameter, calcifications, anatomy of the vessels. In any case, the planning of the suitable landing zone for the endograft placement, ensuring 2cm of intact aorta above the entry point, is fundamental.7 Special consideration should be also given in the identification of anatomical variants such as hypoplastic left or right vertebral artery, dominant left vertebral artery, presence of an aberrant subclavian artery.8
Another point that needs to be mentioned is that sphygmomanometry in both hands uncovered the probable SSS and it may have contributed to the diagnosis even before the presence of symptoms. A simple simultaneous measurement of arterial pressure in both hands, which is an examination without cost or consuming of time, can give important information about the pressure gradient between the vertebral-basilar and the branchial circulations.9
The majority of studies show that the LSA coverage without carotid-subclavian bypass is related to higher risk for neurological complications, as a study including 606 cases from EURO-STAR registry showed.10 On the contrary, a meta-analysis in 1161 patients showed that there was no significant reduction in neurological complications after LSA revascularization implementation11. Kotelis et al. found that the paraplegia rate was lesser in cases that revascularization was not performed compared to the other patients, when LSA was covered.12 According to Scali et al., the determinants associated with spinal cord ischemia are age, aortic coverage length, chronic obstructive pulmonary disease, chronic renal insufficiency and hypertension while no correlation with LSA revascularization was identified.13
According to several studies, the main indications for revascularization of LSA after TEVAR in case of LSA coverage are the presence of dominant left vertebral artery, hypoplastic right or left vertebral artery, incomplete fusion of vertebral arteries in cervical level 1, previous bypass for coronary revascularization with use of internal mammary artery, severe atherosclerotic lesions of the carotids, basilar and vertebral arteries, aneurysm in proximal LSA12,13,14. Moreover, Noor et al. highlight that the length of aortic endograft is a factor that needs to be considered,14 Kotelis et al. strongly indicate revascularization of LSA in patients with dialysis fistula in the left hand, while Ferreira et al. suggest this also in young patients who usually exercise the upper limbs more intensely.15 In any case, the conduction of the carotid -subclavian bypass should be performed carefully as injuries of the phrenic nerve is ob- served in 4,40% of the cases.16 In our department, revasculari- zation of LSA is not performed routinely but it is implemented according to the aforementioned indications.
It is obvious that the main benefit from the coverage of the LSA is the augmentation of proximal landing zone, although there are disadvantages. More specifically, strokes were more frequent in patients without revascularization reaching a percentage of 5,6% while the percentage in cases of revascularization was 3,1% respectively.17 An another research found that the stroke incidence was 8,9%, even after revascularization, and underlined the fact that the carotid-subclavian bypass is a major risk factor that has to be performed selectively.18 Other authors point out that revascularization of LSA reduces the risk of events of acute stroke as it provides the ability of a safe placement of the endograft in close proximity to the ostium of the left common artery. In addition to this, the manipulations at the level of LSA are minimized and this is preventive to embolic events.19 Moreover the majority of authors emphasize on the meticulous control for the exclusion of a postoperative vertebrobasilar insufficiency, which is apparent in 6% of the cases that finally need left subclavian artery revascularization.20
CONCLUSION
As a conclusion, there are numerous concerns in this field and the need of answers is increasing rapidly due to the wide use of TEVAR. One point that is very important in the man- agement of such cases is the careful evaluation of the vertebrobasilar system. When LSCA coverage is performed, high clinical suspicion is required for the early detection of relevant
complications.
DISCLOSURE STATEMENT
We have no conflicts of interest or financial ties to disclose.
References
- Mesar T, Alie-Cusson FS, Rathore A, Dexter DJ, Stokes GK, Panneton JM. A more proximal landing zone is preferred for thoracic endovascular repair of acute type B aortic dis-sections. J Vasc Surg. 2022 Jan;75(1):38-46. doi: 10.1016/j. jvs.2021.06.036. Epub 2021 Jun 28. PMID: 34197944.
- Upchurch GR Jr, Escobar GA, Azizzadeh A, Beck AW, Con- rad MF, Matsumura JS, Murad MH, Perry RJ, Singh MJ, Veeraswamy RK, Wang GJ. Society for Vascular Surgery clinical practice guidelines of thoracic endovascular aortic repair for descending thoracic aortic aneurysms. J Vasc Surg.
- Klocker J., Koell A., Erlmeier M., Goebel G., Jaschke W. et al. Ischemia and functional status of the left arm and quality of life after left subclavian artery coverage during stent grafting of thoracic aortic diseases. J VascSurg 2014;60:64-9.
- Basetti C.,. Chapter 13:Transient loss of consciousness and syncope. In: Aminoff M., Boller F., Swaab D., Jose Bill- er and Jose M. Ferro, eds . Handbook of Clinical Neurology, Vol. 119 (3rd series) , Neurologic Aspects of Systemic Disease Part I, Amsterdam , Elsevier, 2014 p 176
- Lombardi JV, Hughes GC, Appoo JJ, Bavaria JE, Beck AW, Cambria RP, Charlton-Ouw K, Eslami MH, Kim KM, Lesh- nower BG, Maldonado T, Reece TB, Wang GJ. Society for Vascular Surgery (SVS) and Society of Thoracic Surgeons (STS) reporting standards for type B aortic dissections. J Vasc Surg. 2020 Mar;71(3):723-747
- Riambau V, Böckler D, Brunkwall J, Cao P, Chiesa R, et al. Editor’s Choice – Management of Descending Thoracic Aorta Diseases: Clinical Practice Guidelines of the European Society for Vascular Surgery (ESVS). Eur J Vasc Endovasc Surg. 2017 Jan;53(1):4-52.
- Alric P., Canaud L., Branchereau P., Marty-Ané C. , Berthet J. -Ph. Preoperative Assessment of Anatomical Suitability for Thoracic Endovascular Aortic Repair, Acta Chirurgica- Belgica, 2009 109:4, 458-464.
- Janangeer S., Bashir M., Harky A., Yap J.. Aberrant subclavian: new face of an old disease. Vis Surg2018;4:108.
- Toole J., Tulloch F. Bilateral simultaneous sphygmomanometry : A new diagnostic test for subclavian steal syndrome. Circulation Volume XXXIII, June 1966.
- Buth J, Harris PL, Hobo R, van Eps R., Cuypers P. et al. Neurologic complications associated with endovascular repair of thoracic aortic pathology: incidence and risk factors. A study from the European Collaborators on Stent/ Graft Techniques for Aortic Aneurysm Repair (EUROSTAR) Registry. J VascSurg. 2007;46:1103-1111.e2.
- Hajibandeh S, Hajibandeh S, Antoniou SA, Torella F, Antoniou GA. Meta-analysis of Left Subclavian Artery Coverage With and Without Revascularization in Thoracic Endovas- cular Aortic Repair. J Endovasc Ther. 2016 Aug;23(4):634- 41.
- Kotelis D., Geisbusch P., Hinz U., Hyhlik-Dur A., Teng-Ko- bligk H. et al.. Short and midterm results after left sub- clavian artery coverage during endovascular repair of the thoracic aorta. J VascSurg2009;50:1285-92.
- Scali S., Wang K., Feezor R., Huber T., Martin T. et al. Pre- operative prediction of spinal cord ischemia after thoracic endovascular aortic repair J VascSurg2014;60:1481-90.
- Noor N., Sadat U., Hayes P., Thompson M., Boyle J., Management of the Left Subclavian Artery During Endovascular Repair of the Thoracic Aorta. J ENDO- ASCTHER2008;15:168-176.
- Ferreira M.,Monteiro M., Lanziotti L.,Abuhadba G., Ca- portoto L., Deliberate Subclavian Artery Occlusion during Aortic Endovascular Repair: Is it Really that Safe? Eur J
VascEndovascSurg 33,2007 664e667 - Rizvi A., Murad H., Fairman R., Erwin P., Montori V., The effect of left subclavian artery coverage on morbidity and mortality in patients undergoing endovascular thoracic aortic interventions: A systematic review and meta-analysis. J VascSurg2009;50:1159-69.
- Waterford S., Chou D., Bombien R., Uzun I., Shah A. et al.. Left Subclavian Arterial Coverage and Stroke During Thoracic Aortic Endografting: A Systematic Review. Ann ThoracSurg. 2016 Jan;101(1):381-9.
- Scali S., Chang C., Pape S., Feezor R., Bercelli S. et al. Subclavian revascularization in the age of thoracic endovascular aortic repair and comparison of outcomes in patients with occlusive disease J VascSurg2013;58:901-9.
- Bradshaw R., Ahanchi S., Powell O., Larion S., Brandt C. et al. Left subclavian artery revascularization in zone 2 thoracic endovascular aortic repair is associated with lower stroke risk across all aortic diseases. J VascSurg 2017;65:1270-9.
- Lee Teng C., Andersen N., Williams J., Bhattacharya S., McCann R. et al. Results with a Selective Revascularization Strategy for Left Subclavian Artery Coverage During Thoracic Endovascular Aortic Repair. Ann Thorac Surg. 2011 Jul; 92(1): 97-103.


