Preservation of internal iliac artery by using it as target vessel for distal anastomosis of bifurcated aortic grafts during surgical repair of aorto-iliac aneurysms

| Available Online: | January, 2024 |
| Page: | 17-19 |
Author for correspondence:
Nikolaos Kontopodis, MD, MSc, PhD
Vascular Surgery Unit, Department of Cardiothoracic and Vascular Surgery, University Hospital of Heraklion, University of Crete Medical School, PO-Box 1352, 711 10, Heraklion, Greece
Τel: +30 2810392393 / +30 6948202539
E-mail: kontopodisn@yahoo.gr, nkontopodis@uoc.gr
doi: 10.59037/vrfypw81
ISSN 2732-7175 / 2024 Hellenic Society of Vascular and Endovascular Surgery Published by Rotonda Publications All rights reserved. https://www.heljves.com
Abstract
Full Text
References
Images
Abstract
Common iliac artery aneurysms coexist with abdominal aortic aneurysms in 20-30% of cases and may present technical challenges during surgical reconstruction. Rarely, wide iliac bifurcations may be encountered which may render construction of the distal anastomosis in the iliac bifurcation not feasible. In this instance several techniques may be used, but our preferred approach is the anastomosis of the graft in the internal iliac with subsequent transposition of the external iliac artery in the graft limb. We describe this technique in 3 patients. Postoperative course was uneventful with no signs of pelvic or lower limb ischemia and 100% primary patency during 15 months. In conclusion, the anastomosis of the limb of a bifurcated graft with the internal and transposition of the external iliac artery onto the graft limb may simplify aorto-iliac reconstruction in case of wide iliac bifurcations and safely preserve flow in both internal and external iliac arteries.
Full Text
INTRODUCTION
Open abdominal aortic aneurysm (AAA) repair is a major surgical procedure, which presents specific technical challenges when common iliac arteries (CIA) are involved (20-30% of cases).1 Preservation of blood flow to at least one internal iliac artery (IIA) is crucial, since bilateral occlusion is related to a high complication rate, such as buttock claudication, intestinal ischemia and erectile dysfunction.2,3 Typically, in the presence of a CIA aneurysm the distal anastomosis is performed on the iliac bifurcation, including both the orifices of IIA and external iliac artery (EIA). Rarely, this is not technically feasible, either because of the distance between the two orifices or the existence of an aneurysmal IIA orifice. In these cases the technique that has been mainly reported is constructing the distal anastomosis with the EIA and performing a jump graft to the IIA, although data are scarce.4,5 An alternative technique that may be used and simplify the procedure is to anastomose the graft limb with the IIA and then transpose the EIA onto the graft. We present three cases in which this approach was used.
CASE REPORT/TECHNIQUE
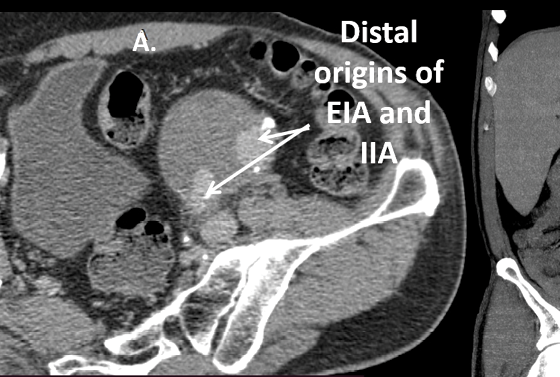
First case regards a 55-year old male patient presenting an aorto-iliac aneurysm with maximum aortic diameter of 87mm, right CIA of 56mm and left CIA of 86 mm. On the left side the origins of EIA and IIA were apart (Figure 1). The patient was treated with open repair, anastomosing the right graft limb with the iliac bifurcation whereas on the left side it was anastomosed with the left IIA and the EIA was transpositioned on the graft limb.
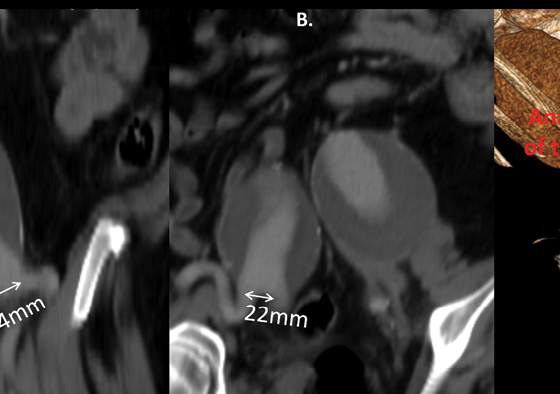
Second case regards a 67-year-old man suffering from a small 40mm AAA, and bilateral CIAs aneurysms with a maximum diameter of 70mm. Figure 2 present the pre-operative CT angiography indicating the long distance between the origins of EIA and IIA in both sides. Figure 2 also displays the postoperative CT angiography indicating ligation of left IIA and anastomosis of the graft to the left EIA while the right IIA was preserved by anastomosing the right graft limb to IIA followed by transposition of right EIA on the graft.
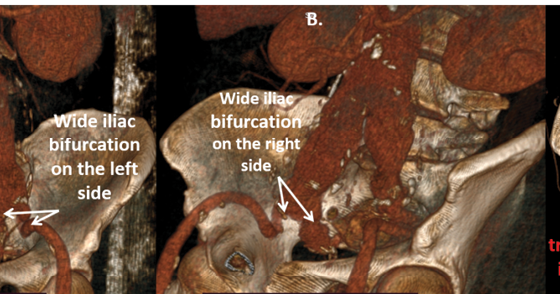
Third case is a patient with a 40mm AAA and bilateral 60mm CIA aneurysms and wide iliac bifurcations bilaterally. Figure 3 presents the pre-operative CT. Figure 3 also displays the 3-Dimensional reconstruction of the postoperative CT angiography with ligation of the right IIA and graft anastomosis to left IIA, and left EIA transposition.
All patients had an uneventful postoperative course. No signs of pelvic or lower limbs ischemic complications were noted. Furthermore, patients presented a free walking ability with no buttock claudication. During a mean follow-up of 15months primary patency of grafts and iliac vessels was 100%.
DISCUSSION
In this report our preferred treatment strategy during open surgical reconstruction of aorto-iliac aneurysms with wide iliac bifurcations is presented. This involves construction of the distal anastomosis in the IIA and subsequent transposition of the EIA onto the graft limb. This approach facilitates the preservation of both IIA and EIA without adding specific technical difficulties in the procedure. In our opinion, the opposite sequence (i.e. construction of the distal anastomosis in the EIA and transposition of the IIA) would be more far more demanding, especially in cases that the IIA lies deep in the pelvis and in a posterior position relative to the EIA. For example, in all three cases reported in the current study (Figures 1A, 2C, 3C) it can be seen that the anastomosis of the IIA origin would be required to be constructed in the posterior side of the graft limb. Therefore, our proposed technique to make the anastomosis of the graft in the IIA and transpose the EIA, may be particularly useful in patients with a deep and posterior IIA location.
Notably, we were not able to identify previous reports on this technique although it is possible that vascular surgeons might use this approach at an empirical fashion. Moreover, we could not retrieve any data on the frequency of an aorto-iliac anatomy that does not allow the inclusion of the EIA and IIA orifices in one anastomosis. According to our experience, this is a rare occasion which was encountered in only 3 cases, among 51 elective aortoiliac reconstructions for AAAs, during a 3-year period. As expected, no specific thresholds to define wide iliac bifurcations exist, but in the current series a distance >2cm between the origins of the division branches was recorded in all 3 cases.
An alternative technique which would be suitable for these cases is external to internal iliac bypass which again has only been scarcely reported in the literature, with most data regarding endovascular treatment of AAAs that need extension of the endograft in the EIA due to wide CIAs.6,7 For these cases, an excellent patency of these grafts has been reported but data are available for a short follow-up of a few months. In our cases during a mean follow-up of 15 months primary patency of grafts and native iliac arteries was universal and no symptoms of pelvic or limb ischemia were reported. Notably, in these patients ligation of the CIA and femoro-femoral bypass in order to ensure reverse flow in the IIA was not feasible due to the distance between the origins of the IIA and EIA. Moreover, it should be underlined that endovascular repair was not preferred in these patients because of their young age and good general health status which made them suitable candidates for open surgery.
In conclusion, the anastomosis of the limb of a bifurcated graft with the IIA and transposition of EIA onto the graft limb is a safe technique to facilitate the preservation of the IIA when anastomosis with the iliac bifurcation is not feasible.
References
- Ziegler P, Avgerinos ED, Umscheid T, Perdikides T, Erz K, Stelter WJ. Branched iliac bifurcation: 6 years experience with endovascular preservation of internal iliac artery flow. J Vasc Surg. 2007;46:204-10.
- Kouvelos GN, Katsargyris A, Antoniou GA, Oikonomou K, Verhoeven EL. Outcome after Interruption or Preservation of Internal Iliac Artery Flow During Endovascular Repair of Abdominal Aorto-iliac Aneurysms. Eur J VascEndovasc Surg. 2016;52:621-634.
- Kudo T. Surgical Complications after Open Abdominal Aortic Aneurysm Repair: Intestinal Ischemia, Buttock Claudication and Sexual Dysfunction. Ann Vasc Dis. 2019;12:157-162.
- Hosaka A, Kato M, Kato I, Isshiki S, Okubo N. Outcome after concomitant unilateral embolization of the internal iliac artery and contralateral external-to-internal iliac artery bypass grafting during endovascular aneurysm repair. J Vasc Surg. 2011;54:960-4.
- Mansukhani NA, Havelka GE, Helenowski IB, Rodriguez HE, Hoel AW, Eskandari MK. Hybrid Endovascular Aortic Aneurysm Repair: Preservation of Pelvic Perfusion with External to Internal Iliac Artery Bypass. Ann Vasc Surg. 2017;42:162-168.
- Kobayashi Y, Sakaki M, Yasuoka T, Iida O, Dohi T, Uematsu M. Endovascular repair with contralateral external-to-internal iliac artery bypass grafting: a case series. BMC Res Notes. 2015;8:183.
- Unno N, Inuzuka K, Yamamoto N, Sagara D, Suzuki M, Konno H. Preservation of pelvic circulation with hypogastric artery bypass in endovascular repair of abdominal aortic aneurysm with bilateral iliac artery aneurysms. J Vasc Surg. 2006;44:1170-5.