Covered Endovascular Reconstruction of Ιnternal Ιliac Bifurcation (CERIΙB)

| Available Online: | September, 2023 |
| Page: | 72-76 |
Author for correspondence:
Konstantinos Spanos, MD, MSc, PhD
Department of Vascular Surgery, University Hospital of Larissa, Faculty of Medicine, School of Health Sciences, University of Thessaly, Larissa, Greece
Email: spanos.kon@gmail.com
Tel.: +306948570321
Fax.: +30-2413501739
doi: 10.59037/hjves.v5i2.4
ISSN: 2732-7175 / 2023 Hellenic Society of Vascular and Endovascular Surgery Published by Rotonda Publications
All rights reserved. https://www.heljves.com
Konstantinos Spanos, MD, MSc, PhD 1 Athanasios Chaidoulis, MD1 Konstantinos Dakis, 1 George Kouvelos, MD, MSc, PhD, 1 Metaxia Bareka, MD, MSc, PhD, 2 Eleni Arnaoutoglou, MD, PhD, 2 Miltiadis Matsagkas, MD, PhD, FEBVS, 1
1 Department of Vascular Surgery, University Hospital of Larissa, Faculty of Medicine, School of Health Sciences, University of Thessaly, Larissa, Greece
2 Department of Anesthesiology, University Hospital of Larissa, Faculty of Medicine, School of Health Sciences, University of Thessaly, Larissa, Greece
Full Text
References
Images
Full Text
INTRODUCTION
Current accepted definition of iliac artery aneurysm (IAA) is the dilatation of the artery > 1.5 times to its normal diameter: common iliac artery (CIA) of > 18-20 mm in men and 15 mm in women, and an internal iliac artery (IIA) of > 8 mm. 1,2 IAAs are commonly associated with the presence of an aneu- rysm in the abdominal aorta (AAA) as aorto-iliac aneurysms rate ranges up to 10% of AAA, while isolated aneurysms of the internal iliac artery (IIAA) are a rare condition (0.4% of all intra-abdominal aneurysms). 1,2 The IIAs’ natural course is not well known because of the lack of evidence describing their natural history, and the fact that many of those are treated in smaller diameters when there is a need for the AAA to be treated; however, most of IIA are becoming larger and rup- ture, leading to significant mortality. 3
Treatment of IIAA is challenging. In many cases, open surgical repair of IIAA poses difficulties due to their deep pelvic localization and, in case of previous open repair of AAA scar tissue may be present. According to the literature, 30-day mortality and complication-rate reach up to 10% and 16%, respectively. 4 Thus, with the EVAR becoming the first choice of AAA treatment, endovascular techniques have been also applied for the IIAA treatment.5 The usual approach is the exclusion of the proximal part of the IIA orifice by deploying a stent graft along the common and external iliac arteries with or without coil embolization of the outflow branches and the IIAA sac itself. In cases where the aneurysm neck anatomy is suitable, an Amplatzer vascular plug has also been successfully used to exclude the arterial inflow and outflow. 3
The main issue of those endovascular techniques is that either unilateral or bilateral IIA occlusion has been shown to carry a risk of significant ischemic complications in nearly one quarter of patients. Especially bilateral IIA occlusion has been related to a significantly higher rate of buttock claudication and even serious ischemic complications regarding the rectum and buttocks. Endovascular techniques have evolved to side branch techniques preserving IIA patency leading to a significant improvement in the treatment of aorto-iliac aneurysms and have been associated with high technical success and low morbidity. 6 Herein, we present a case of treatment of bilateral IIAAs using an off the shelf technique of Covered Endovascular Reconstruction of Internal Iliac Bifurcation (CERIIB).
CASE PRESENTATION AND TECHNIQUE
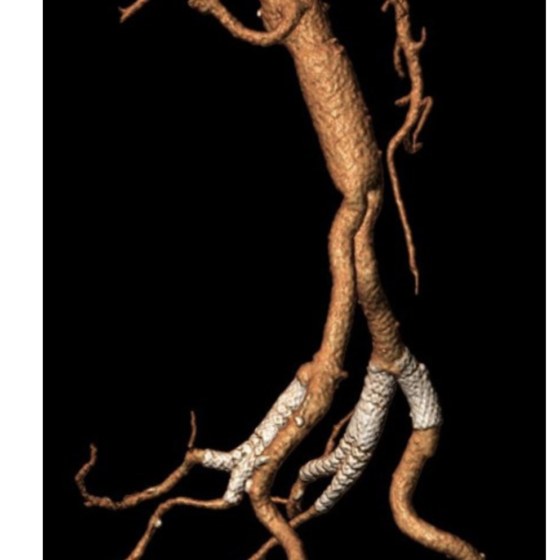
A 67-year-old male had a known history of open surgical repair of an infrarenal AAA 12 years ago. At that time, he underwent an aorto-bi-iliac reconstruction with a Dacron vascular graft from just below the renals to the iliac bifurcations. During follow up, a computed tomography angiography (CTA) revealed bilateral internal iliac artery aneurysms (both sides 30 mm in diameter). (Figure 1) The two possible solutions were overstenting of the orifice of the IIAs with the simultaneous coiling and deployment of a vascular plug of the IIAA in two staged procedures (one for the right and one for the left side), while the other one to attempt a CERIIB technique deploying two parallel balloon expandable covered stents (BXCS) in the outflow branches of each IIA, which would land in parallel fashion inside a previously deployed BXCS in the main trunk of each IIA, similarly to CERAB technique that is being used in the aortic bifurcation
he patient was operated in supine position under general anesthesia. Cut down access was bilaterally used in the superficial femoral artery and in the left axillary artery. Systemic heparinization at 100 IU/kg with a target Activated clotting time (ACT) > 300 s was obtained. A 16 Fr sheath (33mm of length, W.L. Gore & Associates, Flagstaff, AZ, USA) was advanced over an Amplatz guidewire from the axillary artery into the descending aorta for stabilization, and then a long 9 Fr x80mm sheath was inserted up to the right common iliac artery. A 5 Fr Vertebral catheter over a hydrophilic guide-wire was advanced in order to cannulate the right internal iliac artery and one of its two main branches. The wire was exchanged to an Amplatz wire again and a VBX (W.L. Gore & Associates, Flagstaff, AZ, USA) BXCS 11x39mm was implanted in the proximal part of IIA. Leaving the wire in place into the one main distal branch, the catheter was inserted parallel to the wire inside the 9Fr sheath, in order to cannulate the second main distal IIA branch with a hydrophilic wire that was exchanged to another Amplatz guidewire. An angiography from the 9Fr sheath showed the distal landing zone of both IIA branches. The 9Fr sheath was then removed from the 16 Fr sheath, and a first VBX 5x39mm was inserted though the large 16Fr sheath and was appointed in the specific position inside the first IIA branch and inside the previously placed 11mm VBX. Then a second VBX 6x39mm was also inserted from the 16 Fr sheath over the second guidewire in parallel to the previous one, and was also put in place inside the second IIA branch. Both covered stents were then deployed having their proximal part into the 11mm VBX and their distal part into the two main branches. ( Figure 2) After deployment, the balloons of the covered stents were retrieved more proximal outside the IIA branches and another kissing ballooning was undertaken with pressure than the nominal one in order to achieve better formation inside the 11mm VBX and thus to avoid any gutter endoleak
The same technique was exactly used for the aneurysm in the left IIA. ( Figure 3) Again, we deployed a VBX 11x39mm in the proximal part of the IIA and distally a VBX 6x39mm and a VBX 5x39mm in the two main branches of the left IIA, with their proximal part within the 11mm VBX. During the end of this second procedure, we noticed a 50% stenosis in the proximal part of the EIA, caused by a small malposition of the 11mm VBX in the proximal part of the left IIA. Another VBX 11x39mm was deployed ( Figure 4) in the proximal part of the EIA and a kissing stent technique was undertaken (with a balloon just into the IIA stent) with an optimal outcome ( Figure 5). The post-op course of the patient was uneventful and was he discharged at second post-op day on dual antiplatelet treatment for a month. The 1 st month CTA shows exclusion of the aneurysms, with no endoleak or stenosis of the covered stents (Figure 6). All distal branches of both IIAs were patent. The patient is under surveillance on clopidogrel, with a duplex examination scheduled 6 months after the procedure.
DISCUSSION
In this case report we presented the CERIIB technique (Covered Endovascular Reconstruction of Internal Iliac Bifurcation) in a patient with bilateral IIAAs. The CIA is aneurysmal when its diameter exceeds 15—18 mm, and the general threshold for repair is 3 cm. 7,8,9 The challenge of this case was that in both sides large distal branches were present. Someone could argue that an internal iliac branch device may be used, but this would be difficult due to the relative restrictive common iliac diameter, and because it would be necessary to land to one of those branches distally, increasing the risk of IIA occlusion due to poor run off or potential endoleak from the other branch even if it was coiled embolized.
Kim et al. 7 have highlighted that even if endovascular treatment of IIA aneurysms may effectively prevent sac expansion, endoleak was more frequently observed in cases of technical failure and those in which distal IIA branches were embolized. Someone could suggest that there were many other options such as Iliac stent graft deployed over the ostium of the IIA following outflow embolization with or without embolization of the inflow and outflow of the IIA. Technical failure has been associated to incomplete embolization of IIA outflow, and this significantly determines the clinical outcome.7 Additionally, there was a high probability for serious complications due to bilateral IIA occlusion in an otherwise healthy patient, relatively young.
Open surgical techniques include exclusion of the aneurysm sac with proximal ligation alone or in conjunction with distal ligation of the hypogastric artery, formal resection of the aneurysm or proximal ligation of the artery combined with endoaneurysmorrhaphy. 10 In the rare cases of bilateral disease and in order to prevent compromise of the pelvic arterial circulation, an interposition graft may be placed. The deep location of the aneurysm in the pelvic cavity, along with peri-inflammatory tissue reaction, creates considerable difficulties with dissection and aneurysm fixation, the risks of intraoperative hemorrhage are significant, and elective mortality rates of up to 11% have been reported. In emergency cases, the mortality figures may be as high as 50%. 3,11
In terms of clinical impact, literature data described a high rate of buttock claudication (12-19%) and symptoms occurred particularly after the use of coils and especially if they are placed in the outflow branches of the IIA (22-30%). 12,13 Some literature data suggest that coil embolization of hypogastric aneurysm in its distal branches leads to higher rate of buttock claudication and even more serious pelvic ischemia.12,14 On the contrary, claudication is quite rare without coil embolization or after coil deployment in the proximal portion of the vessel. Coils deployment in the vascular district is not a precise procedure, and often the final coil position is changed by multiple forces (blood flow, arterial wall, coil bending). Coils may have been pushed distally by the flow, causing damage at distal arterial vascularization. Even though aneurysm embolization with vascular plugs has not been associated to pelvic complications, still endograft stenosis and thrombosis from vascular plug pressure have been the more frequent complications. 12 Grade of oversize probably plays a fundamental role in the genesis of these complications.
Unilateral or bilateral IIA occlusion during EVAR seems to carry a substantial risk of significant ischemic complications in nearly one quarter of patients. Bilateral IIA occlusion has been related to a significantly higher rate of buttock claudication and serious pelvic ischemia. IIA preservation techniques represent a significant improvement in the treatment of aorto-iliac aneurysms and have been associated with high technical success and low morbidity.
CONCLUSION
CERIIB technique is a novel off the shelf technique that can be used for the treatment of IIAAs with large distal branches, treating the aneurysm and at the same time preserving the blood flow to the pelvic circulation. It requires adequate experience and logistics, and of course needs more evaluation and longer results to be established in the endovascular treatment of IIAAs.
References
- Short DW. Aneurysms of the internal iliac artery. Br J Surg. 1966;53(1):17-20. doi:10.1002/bjs.1800530152
- Kasulke RJ, Clifford A, Nichols WK, Silver D. Isolat- ed atherosclerotic aneurysms of the internal iliac ar- teries: report of two cases and review of literature. Arch Surg. 1982;117(1):73-77. doi:10.1001/arch- surg.1982.01380250051012
- Antoniou GA, Nassef AH, Antoniou SA, Loh CY, Turner DR, Beard JD. Endovascular treatment of isolated inter- nal iliac artery aneurysms. Vascular. 2011;19(6):291-300. doi:10.1258/vasc.2011.ra0050
- Sandhu RS, Pipinos, II. Isolated iliac artery aneurysms. Seminars in vascular surgery.2005;18(4):209-215
- Wanhainen A, Verzini F, Van Herzeele I, et al. Editor’s Choice – European Society for Vascular Surgery (ESVS) 2019 Clinical Practice Guidelines on the Management of Abdominal Aorto-iliac Artery Aneurysms [published correction appears in Eur J Vasc Endovasc Surg. 2020 Mar;59(3):494]. Eur J Vasc Endovasc Surg. 2019;57(1):8- 93. doi:10.1016/j.ejvs.2018.09.020
- Kouvelos GN, Katsargyris A, Antoniou GA, Oikonomou K, Verhoeven EL. Outcome after Interruption or Pres- ervation of Internal Iliac Artery Flow During Endovas- cular Repair of Abdominal Aorto-iliac Aneurysms. Eur J Vasc Endovasc Surg. 2016;52(5):621-634. doi:10.1016/j.ejvs.2016.07.081
- Kim J, Chun JY, Ameli-Renani S, et al. Outcome of endovascular treatment of internal iliac artery aneurysms: a single center retrospective review. CVIR Endovasc. 2022;5(1):53. Published 2022 Oct 18. doi:10.1186/s42155-022-00330-1
- Muradi A, Yamaguchi M, Okada T, et al. Technical and out- come considerations of endovascular treatment for inter- nal iliac artery aneurysms. Cardiovasc Intervent Radiol. 2014;37(2):348-354. doi:10.1007/s00270-013-0689-9
- Kliewer M, Plimon M, Taher F, et al. Endovascular treat- ment of hypogastric artery aneurysms. J Vasc Surg. 2019;70(4):1107-1114. doi:10.1016/j.jvs.2018.12.048
- Philpott JM, Parker FM, Benton CR, Bogey WM, Powell CS. Isolated internal iliac artery aneurysm resection and reconstruction: operative planning and technical considerations. Am Surg. 2003;69(7):569-572.
- Dix FP, Titi M, Al-Khaffaf H. The isolated internal iliac artery aneurysm–a review. Eur J Vasc Endovasc Surg. 2005;30(2):119-129. doi:10.1016/j.ejvs.2005.04.035
- ianchini Massoni C, Freyrie A, Gargiulo M, et al. Perioperative and Late Outcomes after Endovascular Treatment for Isolated Iliac Artery Aneurysms. Ann Vasc Surg. 2017;44:83-93. doi:10.1016/j.avsg.2017.03.194
- Patel NV, Long GW, Cheema ZF, Rimar K, Brown OW, Shanley CJ. Open vs. endovascular repair of isolated ili- ac artery aneurysms: A 12-year experience. J Vasc Surg. 2009;49(5):1147-1153. doi:10.1016/j.jvs.2008.11.101
- Zander T, Baldi S, Rabellino M, et al. Bilateral hypogastric artery occlusion in endovascular repair of abdominal aortic aneurysms and its clinical significance. J Vasc Interv Radiol. 2007;18(12):1481-1486. doi:10.1016/j. jvir.2007.07.034