Repair of Native Infective Aortic Aneurysms. Report of Five Cases and Review of Latin-American Literature

| Available Online: | September, 2023 |
| Page: | 109-104 |
Author for correspondence:
Alberto Muñoz, MD
Chair Vascular and Endovascular Unit,
National University Hospital, Fundación Santa Fe De Bogota University Hospital, Bogota, Colombia
E-mail: alberto.munoz@hun.edu.co
doi: 10.59037/hjves.v5i3.31
ISSN 2732-7175 / 2023 Hellenic Society of Vascular and Endovascular Surgery Published by Rotonda Publications
All rights reserved. https://www.heljves.com
Abstract
Full Text
References
Images
Abstract
Abstract:
Infectious aortitis is a rare disease that rapidly evolves into a false aneurysm and rupture. Antibiotic therapy associated with complete surgical excision of the infected aorta, debridement, and in situ or extra-anatomic revascularization are the most recommended options for infection control and avoiding aortic rupture. However, this surgery has high morbidity and mortality rates, especially in older patients compromised by sepsis, comorbidities and advanced age. This has motivated endovascular repair as a less invasive alternative that has been showing promising results. However, there are uncertainties regarding recurrent or persistent infectious complications. This manuscript describes the management of five patients with primary aortic aneurysm infections, three thoracic and two abdominal. Four were treated endovascularly, and one open. Cases are from Argentina, Colombia, the Dominican Republic and Uruguay. Additionally, a literature review in Latin America is included.
Keywords: Infective native aortic aneurysm, mycotic aortic aneurysm, aortitis, Infected, Aorta.
Full Text
INTRODUCTION
Infectious aortitis is life-threatening, rapidly evolving into a false aneurysm and rupture. Sörelius recommends the term Infective Native Aortic Aneurysm (INAA) instead of mycotic aneurysm since microorganisms are usually bacteria.1 Antibiotic therapy, open repair (OR) with debridement, and in-situ repair with cryopreserved allografts, prosthetic antibiotic-impregnated Dacron, femoral vein or extra-anatomic revascularization, have been the recommended treatment options.2,3 Endovascular aneurysm repair (EVAR) has emerged as a less invasive alternative showing promising results. However, there are uncertainties due to a potentially higher risk of late graft infection. We report five patients treated for INAA and review the Latin America (LA) literature during the past 20 years.
CASE PRESENTATION
Case 1- Montevideo, Uruguay
A 69-year-old man, current smoker with hypertension (HT), presented in May 2010 with enteral sepsis due to Salmonella Species (SS) that was managed with ampicillin-sulbactam and ciprofloxacin. Computed tomography angiography (CTA) showed a horseshoe kidney and two aortic aneurysms of 33- and 35-mm diameter. One month later, CTA revealed aneurysm growth. The patient continued with intense low back pain, raising concern for impending rupture. He underwent EVAR (Figure 1A) with an aortouniiliac graft and femoral-femoral bypass with saphenous vein. Postoperative course was uneventful, and he was discharged on ciprofloxacin after ten days. Eight years later, CTA showed a patent reconstruction without reinfection (Figure 1B).
Case 2 – Bogota, Colombia
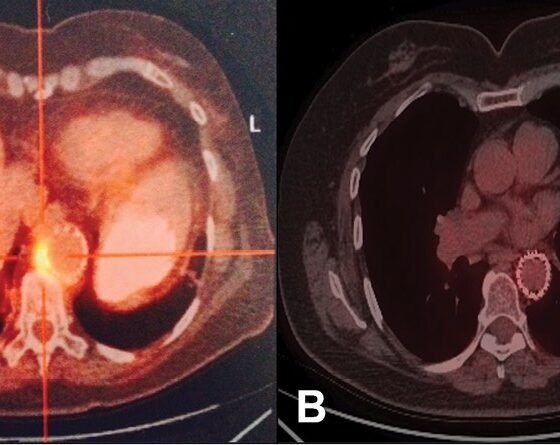
A 67-year-old woman, current smoker and obese, presented in April 2014 with abdominal pain, chills and fever. CTA showed a peri-aortic inflammation and blood cultures positive for SS. Treatment was started with cefepime and meropenem, but severe pain and fever persisted. A CTA two days later demonstrated a false aortic aneurysm one. Thoracic aorta endovascular repair (TEVAR) was performed. PET CT scan revealed abnormal uptake around the endograft (Figure 2A). Antibiotic treatment was continued for six weeks, and the patient was discharged on indefinite ciprofloxacin and rifampicin. Four years later, she was diagnosed with fluoroquinolone enthesopathy, requiring replacement with cefpodoxime. A new PET CT scan showed no aortic uptake (Figure 2B). She died six years later, in July 2021, from COVID-19-related complications.
Case 3 – Santo Domingo, Dominican Republic
A 63-year-old man, current smoker with HT and diabetes mellitus (DM), was admitted in June 2017 with fever, left chest pain, and hemoptysis. Laboratories revealed 23.000 leukocytes/mm3, 29% hematocrit, and 9.6 mg/dL hemoglobin. CTA showed a trilobed thoracic aortic aneurysm (Figure 3A). Emergent TEVAR under local anesthesia was performed (Figure 3B). Blood, urine and bronchoscopic cultures were positive for Klebsiella pneumoniae. Antibiotic therapy with meropenem and fluconazole was continued for eight uneventful weeks and then discharged. Four years later, in December 2021, he presented with fever and massive hematemesis and subsequently died.
Case 4 – Santa Fe, Argentina
A 61-year-old male presented in June 2021 with paraplegia and urinary incontinence caused by a purulent epidural collection. Surgical drainage and laminectomy were performed. Methicillin-sensitive Staphylococcus aureus was isolated and treated with vancomycin and ciprofloxacin. He persisted with fever and hypotension. CTA revealed a pseudoaneurysm in the thoracic aorta located 18.4 mm proximal to the celiac trunk (Figure 4A) successfully treated with TEVAR. After four weeks of antibiotic therapy, pre-discharge CTA evidence complete exclusion of the pseudoaneurysm. In March 2023, he remained free of infectious complications and recovered from paraplegia.
Case 5 – Pasto, Colombia
A 64-year-old male, former smoker, presented in June 2021 with abdominal pain and a liver abscess and was treated with ampicillin-sulbactam and metronidazole. He was readmitted for increased pain and fever. CTA showed a small liver lesion and a saccular infrarenal bilobed false aortic aneurysm (Figure 5A). Blood cultures were positive for Klebsiella pneumoniae, and antibiotic therapy was changed to ertapenem. After three weeks, CTA revealed a left psoas abscess, requiring CT-guided percutaneous drainage. Antibiotic treatment was continued for six weeks until the normalization of inflammatory markers. Then, in-situ repair with debridement and placement of an interposition silver-impregnated Dacron graft covered by pedicled omentum was performed. Intraoperative findings suggested chronic periaortic inflammation and fibrotic changes (Figure 5B). He recovered uneventfully and was discharged on oral ciprofloxacin for four weeks. The patient remains asymptomatic and free of infection.
DISCUSSION
Infectious aortitis is uncommon. In LA literature, we found 12 published cases of INAA (Table 1) in addition to the 5 cases reported in this paper.4-12 The most frequent microorganisms were SS, 5 of 17 (29.4%) and Staphylococcus aureus (23.5%). Patients’ characteristics included age >55 (100%), HT (47%), tobacco use (35.3%) and DM (35.3%). INAAs were found in the infrarenal aorta in 8 patients (47%), descending thoracic 5 (29.4%), suprarenal 3 (17.6%) and arch 1 (6%). EVAR was the treatment in 9 patients (53%), OR in 5 (29.4%) and hybrid repair in 3 (17.6%). OR was mainly used for infrarenal INAAs, whereas EVAR or HR was preferred for thoracic and suprarenal INAAs.
Until 2007, antibiotic therapy and open repair (OR) were considered first line of management with considerable mortality (16-44%). A systematic review from Sorelius, including 28 studies and 963 patients, found that the most common treatment was OR (58%), followed by EVAR (39%) and medical therapy (3%). Before 2010 OR was more common, but lately, EVAR frequency has risen. Postoperative antibiotic treatment >6 months was associated with better survival. Late infections were similar (21%), regardless of treatment approach.3 In LA review we see a tendency to use endovascular treatment plus antibiotics for INAA of the suprarenal and thoracic aorta and OR for the infrarenal.
CONCLUSIONS
INAAs might be underreported in LA. OR is mainly used for the infrarenal abdominal aorta. EVAR or hybrid repair was preferred for the thoracic and suprarenal aorta. Preoperative antibiotics for at least two to six months or lifelong appear to reduce reinfection and graft-related complications.
ACKNOWLEDGMENT
We would like to thank Ana Sofia Acostamadiedo and the Universidad de Los Andes vascular surgery research group VascuAndes for their contribution to data collection.
References
- Sörelius K. Infective Native Aortic Aneurysms: Call for Consensus on Definition, Terminology, Diagnostic Criteria, and Reporting Standards. Eur J Vasc Endovasc Surg. 2020;59:333-334.
- Tabiei A, Cifuentes S, Kalra M, Colglazier J J, Mendes B C, Schaller M Set al. Cryopreserved Arterial Allografts Versus Rifampin-Soaked Dacron For The Treatment Of Infected Aortic And Iliac Aneurysms. Ann Vasc Surg; 2023;92:89-79.
- Sörelius K, Mani K, Budtz-Lily J, Wanhainen A. Systematic review on the management of mycotic aortic aneurysms. Eur J Vasc Endovasc Surg. 2019;58:426-435.
- Patrón M, Russo A, de Sosa F, González Duarte SG, Esperón Percovich A. Experiencia en el tratamiento endovascular de pseudoaneurismas arteriales infecciosos: presentación de tres casos. Angiología. 2021;73(2):95-99.
- González D, Herrera J C, Hasbún S, Tepper P. Manejo de un aneurisma infeccioso. Rev. Cir. 2019;71(5):446-449.
- Vallverdù M, Zeoli M, Icasuriaga A, Andreoli G, Valiñas R. Aneurisma micótico de la aorta abdominal secundario a infección por Proteus mirabilis. Angiología. 2019;71(3):113-115.
- Peralta M, Olguín R, Marín C, Schwartz E. Tratamiento endovascular de aneurismas micóticos de aorta: reporte de tres casos. Angiología. 2018;70(3):132-134.
- Gutierrez-Carreño AR, Lizola-Margolis R, Mendieta-Hernandez M. Aneurisma aorta abdominal micótico roto. Rev Mex Angiol. 2017;45(3):139-142.
- Norese M, Davaro M, Ferreyra S. Aneurisma micótico de la aorta abdominal por Streptococcus pneumoniae. Rev Argent Cardiol. 2013;81:68-69.
- Jimenez C, Valencia A, Jaramillo C, Correa J. Aneurisma aórtico bacteriano por Salmonella spp. Rev Colomb Cir. 2011;26:214-221.
- Sagüés R., Soto S. Manejo híbrido de aneurisma infeccioso de aorta visceral. Caso clínico. Rev Med Chile. 2011;139:1071-1074.
- De Souza E, Muhlethaler C, Ocke P, Borja A. Tratamento de aneurisma micótico da aorta abdominal por Salmonella species com enxerto sintético in situ. J Vasc Br. 2004;3(2):165-8.