Reverse U stent graft technique for the treatment of a type IIIa endoleak with common and internal iliac aneurysms, preserving pelvic flow

| Available Online: | January, 2024 |
| Page: | 26-28 |
Author for correspondence:
Georgios S. Sfyroeras MD
Department of Vascular Surgery, Athens University Medical School, Attikon University Hospital, Rimini 1, 12462, Haidari, Athens, Greece
Τel: +30 6944884621
E-mail: gsfyr@yahoo.gr
doi: 10.59037/v49jpn45
ISSN 2732-7175 / 2024 Hellenic Society of Vascular and Endovascular Surgery Published by Rotonda Publications All rights reserved. https://www.heljves.com
Abstract
Full Text
References
Images
Abstract
Type III endoleak is a severe complication after endovascular aneurysm repair (EVAR) and can result in aneurysm rupture. In the presence of common (CIA) and internal iliac artery (IIA) aneurysm the preservation of at least one IIA is mandatory to avoid pelvic ischemia. A 88-year old man with EVAR extending to the right external iliac artery, presented with a type IIIa endoleak from disconnection between the main body and the contralateral limb. He also had an aneurysm of the left CIA, with subsequent loss of left limb fixation, and an aneurysm of the left IIA, the only one maintaining pelvic flow. A hybrid procedure was performed including placement of an aorto-uni-iliac graft, crossover femoro-femoral bypass and placement of an external to the aneurysmal IIA reverse U stent-graft. Post-operative CT scan demonstrated complete sealing of the endoleak with preservation of pelvic flow through the left IIA.
Keywords: Type III endoleak, Iliac aneurysm, U graft, hybrid treatment.
Full Text
INTRODUCTION
Type III endoleak is a late complication following endovascular repair of aortic aneurysm (EVAR), with incidence ranging from 0.9%-3%1. Although rare, type III endoleak is the second most common cause of late aneurysm rupture, following behind type I endoleaks2. Therefore, it is critical to proceed immediately to treatment upon identification of the problem. An endovascular approach has been the primary choice for treatment of type III endoleaks.3 We present the case of a type IIIa endoleak, in the presence of common (CIA) and internal iliac artery (IIA) aneurysms, in which a standard endovascular technique would present a threat to the patient, as it would jeopardize his pelvic circulation. A consent regarding publication was obtained from the patient.
CASE PRESENTATION
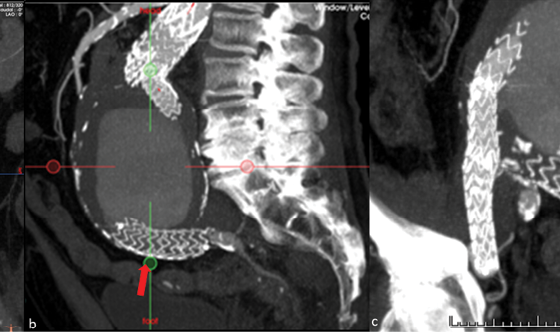
This case refers to an 88-year-old Caucasian male who underwent EVAR in 2010, eleven years prior to the current presentation. His past medical history included hypertension, dyslipidemia, hyperuricemia, and hypothyroidism. He did not comply with his annual post-EVAR follow up for an unknown number of years. A routine abdominal ultrasound revealed an 11 cm aneurysm, and the patient was referred to our department. At presentation, the patient was asymptomatic and his routine laboratory values were within normal ranges. An urgent contrast-enhanced computed tomographic angiography (CTA) scan confirmed the 11cm abdominal aortic aneurysm. The CTA also demonstrated disconnection of the left limb from the main graft body, with loss of distal fixation and aneurysms of both the left CIA artery and the left IIA (3.2cm and 2.4cm respectively). Also, the right limb of the previous endograft was extended to the right EIA (Fig 1).
During multidisciplinary discussion among interventional radiologists and vascular surgeons, the option of a bridging stent graft between disconnected components was rejected, as it would require the graft to land on the left EIA, posing the threat of pelvic ischemia. Instead, an urgent hybrid procedure was planned.
The procedure was performed under general anesthesia with bilateral surgical cut-down for arterial access. Initially, a 36mm TREO aorto-uni-iliac (AUI) endograft (Terumo, Somerset, NJ) was deployed through the right limb of the previous graft (Fig 2). The second step was the construction of a femoro-femoral bypass from right to left using an 8mm PTFE ringed graft. The last planned step would be the placement of a reverse U-stent graft via ipsilateral left CFA access. The initial attempts to advance the stent graft within the IIA failed due to the steep angulation of the IIA origin and the insufficient support due to the largely aneurysmal CIA. A molding balloon, which temporarily sealed the left CIA, facilitated insertion of a 0.035’ stiff hydrophilic guidewire (Terumo, Japan) deep within the left aneurysmal IIA before the deployment of the reverse U-stent (Viabahn 8X100 mm and 10×50 mm) (Fig 3). Completion angiography demonstrated the complete exclusion of all three aneurysms without any signs of endoleak. Aneurysms’ exclusion without endoleak was also confirmed at 1-month follow up CT angiography.
DISCUSSION
This is the first report of a type IIIa endoleak and a IIA aneurysm treated using a hybrid surgical and endovascular AUI and reverse U stent technique.
Type III endoleaks include the IIIa and IIIb subtypes.4 Subtype IIIa is the result of disconnection between one limb and the main body of the stent graft, while subtype IIIb is the consequence of a fabric defect. In this case, the existence of aneurysms in the left common and internal iliac artery likely contributed to the loss of left limb fixation, whilst making the treatment approach more complex.
Treatment of type IIIa endoleaks includes the vastly favorable minimal invasive endovascular treatment, as well as open surgery, which is more dangerous, especially in patients of advanced age with various comorbidities, as in this case.5
The usual endovascular treatment for type IIIa endoleak is an actual reconnection of the disconnected components using a stent graft. However, as the newly inserted stent should land on a healthy artery, the option for our patient would be to land the stent graft at the left EIA, completely excluding the left IIA and posing the patient to the risk of pelvic ischemia.
The proposed use of an AUI stent graft and femoro-femoral bypass is a well-established procedure7 and the placement of a reverse U-stent graft from the EIA to the IIA has been used in the past in certain occasions to prevent retrograde flow into the aneurysmal sac.7,8
In the herein presented case the challenge was to treat simultaneously both the type IIIa endoleak and the IIA aneurysm, as the IIA was the only vessel providing perfusion to the pelvis. Due to the acute angulation of the IIA origin, the advancement of the stent graft within the IIA was not possible even with the use of a super stiff 0.035’ guide wire. Therefore, after placing a stiff hydrophilic guide wire deep within the IIA, a CIA occlusion technique with a molding balloon was used to occlude the aneurysmal CIA and provide support for the advancement of stent graft across the IIA origin, and distal to the aneurysm, as to achieve efficient exclusion.
A valid alternative endovascular treatment option would be the use of an iliac branched stent graft. However, bridging of the disconnected left limb, advancing the stent graft through the bifurcated graft and deployment of the bringing stent graft would be extremely challenging in this particular anatomy. Due to the same anatomical reasons, a periscope stent graft to the left IIA was also rejected as a possible option. Also, the possibility of recurrent disconnection and new type IIIa endoleak that would threaten any further treatment could not be excluded.
In the preoperative CT scan the inferior mesenteric artery was occluded. Also no patent lumbar arteries were noted. Based on these CT findings we decide not to place coils in the aorta and the common iliac artery aneurysms to eliminate any type II endoleak causing further sac expansion. Completion angiography did not demonstrate a endoleak and we decided not to perform any additional interventions.
To conclude, our hybrid technique resulted in safe and successful treatment of a complex type IIIa endoleak. Such a technique may therefore be considered when standard endovascular treatments are not an option.
References
- Chang RW, Goodney P, Tucker LY, et al. Ten-year results of endovascular abdominal aortic aneurysm repair from a large multicenter registry. J Vasc Surg. 2013 Aug;58(2):324-32
- Antoniou GA, Georgiadis GS, Antoniou SA, et al. Late rupture of abdominal aortic aneurysm after previous endovascular repair: A systematic review and meta-analysis. J Endovasc Ther. 2015;22(5):734-44.
- Eng ML, Brewer MB, Rowe VL, Weaver FA. Treatment options for late type III endoleaks after endovascular aneurysm repair. Ann Vasc Surg. 2015;29(3): 594.e5-9.
- Chaikof EL, Blankensteijn JD, Harris PL, et al. Reporting standards for endovascular aortic aneurysm. J Vasc Surg. 2002 May;35(5):1048-60.
- Maleux G, Poorteman L, Laenen A, et al. Incidence, etiology, and management of type III endoleak after endovascular aortic repair. J Vasc Surg. 2017;66(4):1056-64.
- Bergamini TM, Rachel ES, Kinney E V., Jung MT, Kaebnick HW, Mitchell RA. External iliac artery-to-internal iliac artery endograft: A novel approach to preserve pelvic inflow in aortoiliac stent grafting. J Vasc Surg. 2002;35(1):120-4.
- Hoffer EK, Nicholls SC, Fontaine AB, Glickerman DJ, Borsa JJ, Bloch RD. Internal to external iliac artery stent-graft: A new technique for vessel exclusion. J Vasc Interv Radiol. 1999;10(8):1067-73.
- Kotsis T, Tsanis A, Sfyroeras G, Lioupis C, Moulakakis K, Georgakis P. Endovascular exclusion of symptomatic bilateral common iliac artery aneurysms with preservation of an aneurysmal internal iliac artery via a reverse-U stent-graft. J Endovasc Ther. 2006;13(2):158-63.