Contemporary Role of IVC Filters and Advanced Retrieval Techniques

| Available Online: | April, 2024 |
| Page: | 41-48 |
Author for correspondence:
Tsirigoti Alexandra
Department of Vascular Surgery, National and Kapodistrian University of Athens, “ATTIKON” Universitry Hospital, Athens, Greece
Τel: +30 2810392393 / +30 6948202539
E-mail: alexandratsirigoti@gmail.com
doi: 10.59037/1h40xk83
ISSN 2732-7175 / 2024 Hellenic Society of Vascular and Endovascular Surgery Published by Rotonda Publications All rights reserved. https://www.heljves.com
Alexandra Tsirigoti, MD1, Vasileios Bouris, MD2, Efthymios Avgerinos, MD1,2,3
1 Department of Vascular Surgery, University of Athens, University General Hospital “ATTIKON”, Athens, Greece
2 Department of Vascular and Endovascular Surgery, Athens Medical Center, Athens, Greece
3 Department of Vascular Surgery, University of Pittsburgh Medical Center
Abstract
Full Text
References
Images
Abstract
Abstract:
The role of inferior vena cava filters (IVCF) has been controversial over the years, due to concerns regarding their overuse for non-specific indications. Current guidelines recommend their use for patients with proximal deep vein thrombosis who have contraindications or have failed anticoagulation therapy. Prophylactic placement while occasionally justified, remains controversial as robust evidence is lacking. Decision making regarding any IVCF application should be based on a thorough patient selection, ‘cost-effectiveness’ evaluation of the procedure and a proper follow-up protocol needs to be in place for retrieval. A variety of different types and designs of mainly retrievable IVCF is available. The IVCF should be removed when their use is no longer indicated. Prolonged dwell time is not only linked with filter-related complications, but can also lead to a challenging retrieval and/or failure. Advanced filter retrieval techniques are currently available with excellent results, even under complicated circumstances, when performed by experienced physicians.
Keywords: IVC filter, IVC filter complications, IVC filter indications, IVC filter retrieval, Pulmonary embolism, Deep vein thrombosis
Full Text
INTRODUCTION
Deep vein thrombosis (DVT) and pulmonary embolism (PE), combined known as venous thromboembolism (VTE) are the third cause of cardiovascular death after myocardial infarction and stroke.1 The reported annual incidence of DVT in the United States is 80 cases per 100,000 people, more than 60% of which, will develop PE. Although PE is usually asymptomatic, it is a complication of DVT that can lead in hospitalization, with high morbidity and mortality rates.2 The “gold standard” treatment for patients with DVT and/or PE, is anticoagulation (AC) therapy. However, for a high-hemorrhagic risk patient with existing or at risk of VTE, AC therapy is contraindicated.3 In particular, in cases of intracranial bleeding or other major bleeding, active gastrointestinal bleeding, threatened abortion, preeclampsia and eclampsia, malignant hypertension, brain surgery and spinal surgery, AC therapy is contraindicated, as identified by ICD-9-CM diagnosis or procedure codes.3 The need to prevent the occurrence of PE in those patients, supports the use of either permanent or retrievable inferior vena cava filters (IVCF).1
The American Heart Association4, the Society of Interventional Radiology (SIR)5,6, and the American College of Radiology7 have supported the use of IVC filters over the years. However, with only a few studies of adequate strength proving evidence for their efficacy, controversy amongst medical communities and experts has been provoked.8 More recently, the SIR and the Society for Vascular Surgery (SVS) jointly announced the publication of the “Predicting the Safety and Effectiveness of Inferior Vena Cava Filters (PRESERVE)” study, the largest prospective study undertaken regarding outcomes with contemporary IVCF use. The results demonstrated that IVCF are safe and effective for the treatment of VTE, able to prevent DVT from developing into PE.9
However, the main concern of experts and scientific boards remains on whether the advantages of the placement of an IVCF, can outweigh potential complications particularly when filters dwell for long periods; and then which is the safest choice for the patient: to perform a challenging IVCF retrieval or rather leave it behind.
Aim of this review is to summarize the current evidence regarding the use of IVCF, and report the latest trends in IVCF retrieval techniques highlighting potential challenging parameters of the procedure.
IVCF studies
PREPIC studies
According to the first ever randomized controlled trial PREPIC and its 8-year follow up, the placement of an IVCF to a patient that can receive proper AC therapy, does not benefit neither the short nor the long term patients’ survival. More specifically, in a series of 400 patients with acute PE and a high risk of recurrence, the PREPIC study compared the safety of retrievable vena cava filters plus AC, to AC therapy alone. After a two-year follow up period, no significant differences in symptomatic PE or survival between the two groups were observed, apart from a higher rate of DVT recurrence in the patients of the IVCF group (20.8% vs. 11.6%, P=0.02). At 8 years of follow-up, patients with IVCF had a smaller rate of symptomatic PE (6.2% vs. 15.1%, P=0.008) but a significantly higher incidence of DVT (35.7% vs. 27.5%, P=0.042). The overall incidence of VTE, post-thrombotic syndrome and mortality was similar among the 2 groups. Authors came to conclusion, that systematic use of IVCF in patients with VTE who can be treated with anticoagulants, is not recommended. Ιt is suggested though, only in case of failure or contraindication of AC therapy.10,11
PREPIC2 a randomized, open-label, blinded end point trial with 6-month follow-up, conducted from August 2006 to January 2013 compared the results from hospitalized patients with acute, symptomatic pulmonary embolism associated with lower-limb vein thrombosis and at least 1 criterion for severity that underwent to retrievable inferior vena cava filter (RIVCF) implantation plus AC (filter group; n = 200), with patients that received AC therapy alone with no filter implantation (control group; n = 199). In the filter group, the filter was successfully inserted in 193 patients and was retrieved in 153 of the 164 patients in whom retrieval was attempted. Follow-up after 3 months showed recurrent pulmonary embolism occurrence in 6 patients (3.0%; all fatal) in the filter group and in 3 patients (1.5%; 2 fatal) in the control group (relative risk with filter, 2.00 [95% CI, 0.51-7.89]; P = .50). The results were similar at 6 months and indicated that the use of a RIVCF plus AC compared with AC therapy alone did not reduced the risk of symptomatic recurrent pulmonary embolism at 3 months and therefore a RIVCF is not recommended for patients who can be treated properly with AC.11
Further investigation however, needs to be done towards the placement of temporary IVCF, in selected patient groups, that are prone to develop VTE and unable to receive prophylactic AC therapy.
PRESERVE study
Recently, the “PREdicting the Safety and Effectiveness of InferioR VEna cava filters (PRESERVE)”, a prospective, nonrandomized study at 54 sites in the United States between October 10, 2015, and March 31, 2019, demonstrated that the IVC filters are both safe and effective when used to prevent the clinically significant PE. The study enrolled 1429 participants (53.3% male), IVCF were implanted in 1421 patients and were evaluated at baseline and at 3, 6, 12, 18, and 24 months. The follow up for the patients whose IVCF were removed, was for 1 month after retrieval. Of these, 71.7% had current DVT and/or PE. AC therapy in 81.6% was contraindicated or had failed. 8.9% of the implanted IVCFs were prophylactic. IVCF were removed from 44.5% of the patients at a median 86.3 days following implantation, of which 96.8% at first attempt. The primary safety endpoints (freedom from perioperative serious adverse events (AE) and from clinically significant perforation, VCF embolization, caval thrombotic occlusion, and/or new deep vein thrombosis DVT within 12-months) and primary effectiveness endpoints (composite comprising procedural and technical success and freedom from new symptomatic PE confirmed by imaging at 12-months in situ or 1 month postretrieval) were both achieved.
Procedural AEs were rare and not severe and VCF-related AEs were uncommon. One patient died during attempted IVCF removal. Postfilter, venous thromboembolic events (none fatal) occurred in 6.5%, including DVT (5.2%), PE (1.6%), and/or caval thrombotic occlusions (1.1%). No PE occurred in patients following prophylactic placement.
These results might at first seem in favor of the use of IVCF, taking also into consideration the high rate of IVCF removal, however they are overshadowed by study’s limitations. It is worth mentioning that the PRESERVE study is not randomized and the majority of the enrolled patients were in severe health state, with limited therapeutic alternatives and contraindication to the optimal AC therapy. As the authors state “withholding AC therapy from control groups with VTE is an unethical deviation from standard of care”.9
Moreover, the broad inclusion criteria used in the study don’t clarify the potential effect of concomitant AC therapy, the patients may have received prior, at the time and after the placement of IVCF and also the severity of VTE of the patients at presentation. VTE events or PE that occurred only a short period of time after the IVCF placement can be attributed to pre-existing DVT or PE. In other words, the study does not separate high and low risk patients, and how this might have impacted the results, was not sufficiently considered in the analysis.
It is challenging to determine if the placement of an IVCF generates any net benefits without a control group. Whereas there is no proven evidence for claiming the success of the intervention (filter implantation) without comparing it to optimal medical care and other forms of thromboprophylaxis. Yet, despite these limitations, placement of an IVCF was deemed relatively safe and effective.
IVC Filter Indications
According to the ESVS (2021) Clinical Practice Guidelines, temporary inferior vena cava filter insertion is recommended and constitutes the only viable treatment option, for patients with proximal deep vein thrombosis who have contraindications to anticoagulation during the initial or principal treatment phase (Class I / Level C).12 Nevertheless, for a patient properly receiving AC treatment, the routine use of an IVCF is not recommended (Class III / Level B).12 IVCF can’t treat and prevent VTE, but they can prevent the serious complication of PE.
As a relative indication an IVC filter can also be considered in AC treatment failures8,12 and selectively in percutaneous endovenous interventions.13,14,15
Prophylactic use (absence of active VTE) in high risk groups (e.g. polytrauma, spine or bariatric surgery) has also expanded over the past several years given their ease of use, however it remains highly controversial. A multidisciplinary decision weighing costs and benefits is necessary. As awareness on IVC filter potential complications has increased, the prophylactic use is declining.16,17,18
All indications are summarized in Table 1.
Role of Permanent vs Retrievable IVCF
Permanent IVCF currently in use include Vena Tech LP (B. Braun IS, Bethlehem, PA), titanium Greenfield (Boston Scientific, Watertown, MA), Trap Ease (Cordis, Bridgewater, NJ), Simon Nitinol (Bard Peripheral Vascular Inc., Tempe AZ), and Bird’s Nest (Cook Group, Bloomington, IN) filters. Although permanent IVCF are not designed to be removed from a percutaneous approach, they can be removed, if needed, at specialized centers capable to perform advanced retrieval techniques (ART).
Retrievable IVCF on the other hand, permit percutaneous removal if and when the risk of PE resolves. They are designed to be maintained in place in the IVC by hooks, barbs, or radial pressure. Among many examples are Celect (CookMedical Inc, Bloomington, IN), Günther-Tulip (Cook Medical Inc), Option (Argon Medical Devices, Athens, TX), ALN (ALN Implants Chirurgicaux, Ghisonaccia, France), Denali (and predecessors Meridian, Eclipse, and G2) (Bard Peripheral Vascular Inc.), Tempofilter II (B. Braun, Melsungen, AG), G2 and G2x (Bard Access Systems Inc., Salt Lake City, UT, USA) and Crux (Volcano Corp, SanDiego, CA).19
All IVCF have FDA approval for permanent use. This only constitutes one parameter of the low retrieval rates, not matched by the corresponding growth in removable IVCF implantation.19 RIVCF and their flexible indications may sound appealing given the operators ability to postpone decision-making, regarding the optimal removal time, however permanent IVCF for a patient with a prolonged or lifelong need for protection may seem to be a better choice (Figure 1).19 According to Brothers et al. analysis, permanent filters had greater predicted effectiveness compared with RIVCF implantation (5.41 quality-adjusted life-years [QALY] vs 5.33 QALY) at a lower cost ($2070 vs $4650).20 Also the implantation of RIVCF according to the literature has a higher rate of complications and greater percentage of adverse events after prolonged dwell time. A retrospective single center study of 1234 IVCF placed from 2005 to 2010 explored the differences in patients’ characteristics and complications between those with retrievable (group A) and those with permanent filters (group B). The complication rates were significantly higher in the group of indwelling RIVCF, than the group with permanent filters (9% vs 3.0%; P < .0001) after mean follow-up of 20 months. Both thrombotic and device-related complications were more common with retrievable filters, and therefore their long term use should be avoided.21
According to an analysis of filter data from a single institution, whether an optional IVCF can become permanent can be quantitatively predicted from patient parameters. Advanced age, male sex, history of underlying malignancy, and history of anticoagulation failure are positively correlated with optional filters being declared permanent.22 It is important to emphasize that retrievable filter use should be limited to patients with appropriate indication for filter placement in whom retrieval is highly likely and feasible. Retrievable filters are designed to allow the filter to be easily collapsed during retrieval like an umbrella, in comparison with permanent filter designs characterized of a more durable structure.21 Physicians should make their decisions regarding the placement of a permanent IVCF based on each patients’ individual criteria, their risk for PE, and their potential need of life-long protection. Since there are no RCTs published yet to compare permanent and retrievable filters, widely acceptable guidelines and recommendations are still not available.19
Filter related Complications
Whether the benefits from an IVCF placement can outweigh potential complications, is in association with the patients’ unique characteristics and available treatment options. As already mentioned in the PREPIC study, the patients at the IVCF plus anticoagulation group showed a higher rate of DVT recurrence comparing to those treated only with anticoagulation alone.11 A retrospective cohort study, of 126 030 patients with VTE, 45 771 (36.3%) were treated with an IVCF, whereas 80 259 (63.7%) did not receive a filter, after adjustment for immortal time bias, showed that IVCF placement in patients with venous thromboembolic disease and a contraindication to anticoagulation was associated with a significantly increased hazard ratio of 30-day mortality (1.18; 95%CI, 1.13-1.22; P < .001).3
Prolonged IVCF dwell time can cause IVC thrombosis, IVC penetration, filter migration, DVT and filter fracture.23 The FDA-approved IVCF types have device-specific risks. Better understanding of the complications each filter may cause, can help identify patients who may benefit from ongoing follow-up instead of a filter retrieval.24 Risk of penetration is higher with purely conical filters (90-100%). Filters with cylindrical or umbrella elements are associated with the highest reported risk of IVC thrombosis (30-50%), whereas earlier generation filters are associated with high risk of fracture (40%).24 A limitation of the reported device-specific complications, is the lack of equal follow up duration for the used devices among the available studies, considering also that complications tend to increase after longer dwell times.24
Optimal time for retrieval
IVCF with prolonged dwell time that are no longer indicated for use, should be evaluated for removal, in view of the risk of long-term IVCF complications described in the previous section.
Considering the FDAs’ recommendations, a retrievable filter should be removed when protection for PE is no longer indicated. In fact, only a small percentage of them are removed, which varies between studies, but the majority of RIVCF are left in place permanently, with early reported retrieval rates as low as 8.5%.25 This can be attributed to physician oversight and patients’ noncompliance with the follow up protocol. However, according to Avgerinos et al., appropriate rigorous follow up protocols have improved retrieval rates to 60-70% at best.26
Prolonged dwell time is associated with a potentially challenging retrieval procedure. Filter retrieval is defined as challenging when retrieval is unsuccessful due to technical failure or when adjunctive endovascular maneuvers or access sites are necessary to achieve filter removal.26 According to Avgerinos et al. filter retrieval can be challenging or fail when the dwell time is >50 days and >90 days, respectively, and when the filter hook opposes the caval wall.26 Desai et al. suggested that patients with RIVCF in place beyond 7 months, may face difficulties during retrieval, with a calculated risk of standard technique failure at 40.9%, and a referral to centers with expertise in advanced filter retrieval techniques is the best option.27 In a single center study of 648 retrievals, technical success was achieved with standard retrieval techniques in 536 procedures (82.7%); with adjunctive techniques, 631 (97.4%) whereas dwell time (52/648 with dwell time > 6 months) did not affect technical success (OR, 0.98 [95% CI, 0.95-1.01]; P = .12).28
Filter retrieval techniques
Standard retrieval technique (SRT) is performed with the use of a snare and a coaxial sheath.29 The endovascular snare device is used in order to capture the filter apex/hook. Firstly, a cavography is performed in order to examine potential in situ filter thrombus, then telescopic sheaths are placed right adjacent to the filter. When the hook is captured, opposite traction is applied to both the snare and sheath to remove the RIVCF from the caval wall.30
Any other technique that requires additional tools to achieve filter removal is considered advanced.29 In the literature ART were classified as stiff wire displacement, loop snare realignment, wire loop and snare sling technique, wire and snare flossing, balloon displacement, parallel wire and dual sheath, and dissection with off-label tools (endobronchial forceps).29 Avgerinos et al. reported an overall success rate of 91.5% and a 71.1% success rate with advanced techniques. Al-Hakim et al. reported 73.2% success using standard techniques and 94.7% success with advanced techniques. Dowell et al. also reported a 65% success rate using advanced techniques and overall success rate of 96.5%. This can be attributed to the operator’s comfort using the optimal ART.29 Limitations of the published studies are among others, that the type of each ART used in not objectively assigned and is utilized based on the operators skills and preference.29
Advanced retrieval technique vs difficult retrieval scenario
Curved inner sheath
The majority of the available filter designs have a conical shape, which allows them to adjust to the caval wall, at one “circle” formed by the peripheral ends of the device. Filter tilt occurs when external anti-parallel force is applied to the long axis of the filter.25 As a result of the tilt, the filter may not be adequate to capture a thrombus or its position will lead to easier thrombus formation. Standard straight sheaths and snare devices are often unable to successfully capture the filter hook in order to achieve retrieval. A curved inner sheath can facilitate successful snaring of a hook that is significantly deviated from the central axis of the IVC. Desai et al. suggests the use of a Flexor Ansel Guiding Sheath with Ansel 2 modification (Cook Medical) to provide additional directionality in securing a tilted filter.25
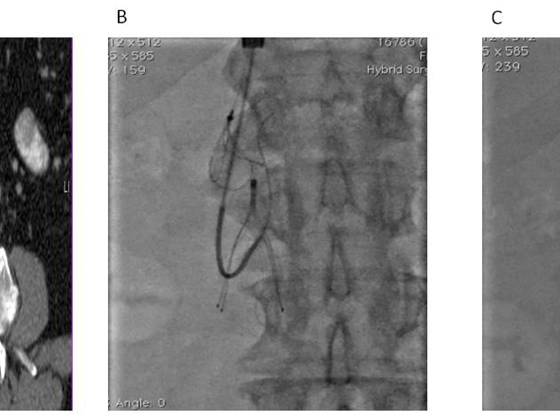
Loop – snare technique
In case of filter tilt, the filters hook/apex is located in close apposition with the caval wall which results to significant blood flow disruption, leading to development of intimal hyperplasia and endothelialization.25 As a result, the hyperplastic tissue which is formed and covers the hook constitutes a challenging retrieval. The basic principle of the loop-snare technique is to capture a tilted or embedded filter via forming a wire loop through the main body of the RIVCF,30 by passing a wire between at least two filter legs/struts and then snaring it superiorly to create the loop, which engages the filter for retrieval (Figure 2).31 This technique may fail in cases with an embedded hook.31 According to Desai et al., a modified technique that targets the fibrin cap is used, in which a reverse-curve catheter aids to engage the radiolucent hyperplastic cap encasing the filter apex. A hydrophilic wire is then passed cranially and snared, forming a wire loop through the tissue cap. The sheath is then advanced coaxially over the wire loop, resulting in either capture and collapse of the filter or disruption of the tissue cap. Then, a standard snare is used to capture and retrieve the filter.25
The modified loop-snare technique that creates a wire loop between the filter neck and the IVC wall, for release of embedded filter hooks is referred to as “The hangman technique”.32 The Hangman technique is described by Al-Hakim et al. and is performed as follows; A right-sided internal jugular vein approach is used with placement of a 14-F x 45 cm sheath (special order; Cook, Inc). A 16 or even an 18Fr sheath can be more efficient. Through this sheath, a 5-F reverse curve catheter (SOS Omni Selective Catheter; AngioDynamics, Latham, New York) is advanced distal to the filter and a glidewire is brought down, around and up above the filter neck to be snared using a 25-mm Amplatz GooseNeck Snare (ev3 Endovascular, Inc, Plymouth, Minnesota) and with-drawn through the sheath. The reverse curve catheter is withdrawn, and cranially directed tension is applied to both the leading end and the trailing end of the wire to release the embedded filter hook from the IVC wall and align it with the sheath and remove it. In cases when filter neck cannot align with the sheath, the double wire system can be rotated creating a spiral that aligns the filter with the sheath and then the sheath can be pushed down and filter can be removed. It is important to understand that high forces may be needed to remove the filter and this is safe provided that these forces are applied against the sheath and not against the IVC wall.
Al-Hakim et al. reported a retrieval success rate of 81.9% (9 of 11 cases; mean tilt, 13.3 degrees +/- 3.9 and an embedded hook (mean dwell time, 194.5d)) and no associated complications.31 A low-profile hangman technique, with the use of a standard 11 Fr Cook filter retrieval sheath, in 23 patients was successful on initial attempt in 22 cases (96%), median dwell time was 196 days, and no procedure-related complications occurred.32
Endobronchial forceps
Rigid Endobronchial forceps are used off-label for filter retrieval; however, they can be safely and reliably used to remove not only embedded, but also fractured, or tilted RIVCF from patients in whom SRT were unsuccessful.33 Endobronchial forceps are usually malleable and can be shaped to provide the appropriate degree of curvature to reach an embedded filter hook, achieve dissection of the tissue from the filter apex and finally centering the filter and allow retrieval with a standard snare or alternatively with the forceps itself.25 With the use of forceps, physicians should be careful for potential caval distention or laceration of the caval wall.
According to a single-center retrospective review, in 60 consecutive patients, 58 IVCF were successfully retrieved with rigid endobronchial forceps. Filter fractures intra-operatively occurred in 10 patients, and four complications were reported, including 1 retroperitoneal hemorrhage, 1 IVC flap, and 2 filter component migrations, both of which were retrieved with a snare device.33 Another single-center retrospective series reported 114 patients with tip-embedded optional IVCF of a variety of models, with median dwell times 465 days. Filter retrieval was successfully achieved in 109 of 114 (96%) patients with the use of a 12-14Fr sheath combination.34 The same institution in a subsequent study evaluated the use of a larger 16Fr sheath, for retrieving “closed-cell” filters, which have a higher incidence of strut and wall-embedment, in 35 patients and found 100% technical success rate in retrieving Gunther Tulip (CookInc,Bloomington,IN), Option (Argon Medical Devices, Plano, TX), and Opt Ease (Cordis Endovascular, Warren, NJ) IVCF.35 Insignificant caval spasm and filling defects were observed in 17 of 34 patients, but there were no major adverse events, which further highlights the benefits of the stiffer and larger 16-Fr sheath for dissecting the heavily embedded filter elements from the caval wall, providing stable forward counterforce.35 After more than a decade since the first description of forceps-assisted IVCF retrieval in 2006, with increased operator experience, the fluoroscopy times required for the retrieval have dropped to less than a median of 10 minutes. As endobronchial forceps can be sterilized and reused, the cost of a forceps-assisted retrieval is much less compared to many other advanced retrieval techniques.36
Laser ablation sheaths
RIVCF with prolonged dwell times can become embedded to the caval wall, due to vascular remodeling and neo-intimal hyperplasia. As a result, the filter cannot be removed with a standard sheath and the use of additional force could cause more damage.30 Laser ablation sheaths, originally designed for pacemaker lead extraction, have been successfully used “off-label” to photothermally ablate neointimal tissue encasing the filter struts within the caval wall, allowing filter removal.25 Kuo et al. after failed retrieval using 3X standard force, were able to remove 98% of embedded filters utilizing the laser sheath technique. In particular, by placing a laser sheath (Spectranetics) connected to a 308-nm XeCl excimer laser generator (CVX-300, Spectranetics), to achieve fibrotic tissue ablation.37 The major complication rate was 2.0%, and all were successfully treated with either medical management and/or percutaneous endovascular therapy. IVC hemorrhage occurred in three patients (0.6%) (3/500) and was attributed to laser activation, at the time when the laser sheath wasn’t safely centered within IVC lumen.37 Desai et al. reported that filters with a “Closed-cell” design (Gunther Tulip (Cook, Inc, Bloomington, IN), Option and Option Elite (Argon Medical Devices, Inc, Plano, TX), OptEase and TrapEase, and Simon Nitinol (Bard Peripheral Vascular, Tempe, AZ), may necessitate the use of the laser sheath for higher rates of successful and safe retrieval when compared with “open-cell” filters (odds ratio, 20.1). In their study the laser sheath was required in 143/441 cases in total (mean dwell times for all filters was 56.6 months) with technical success 96% (134/143). To achieve successful retrieval of closed-cell filters, laser-sheath assistance was necessary in 127 of 210 (60.5%) of cases as compared with open-cell filters that requiring the laser sheath in 16 of 231 (7.0%).38 One complication occurred among laser sheath retrievals and required short admission for a femoral access site hemorrhage.38
Novel Filter Designs
New and improved retrievable VCF devices are constantly developed targeting smaller delivery systems, non-tilting configurations, improved stability, safety while indwelling, aiming to reduce complication rates and reassure an easier retrieval procedure. New designs have recently been made commercially available in Europe (e.g. VIDI Vena Cava Filter, Veniti Inc, MO, USA; Angel Catheter, BiO2Medical Inc, CO, USA).
An innovation and potentially the future of IVCF, is the creation of absorbable filters. Studies have been made regarding the development and in vitro testing of several absorbable vascular filter designs and materials that could possibly erase the long-term complications of conventional IVCF and eliminate filter retrieval.39 The feasibility, effects, and complications of a resolvable IVCF also was tested in vivo to animal models, but further research of bioabsorbable polymers, absorption mechanics in the vascular system, and absorption times needed to be done.40
In a recent non-randomized prospective multicenter trial, the Sentry bioconvertible IVCF was implanted in 129 patients with documented DVT and/or PE (67.5%) or who were at temporary risk of developing DVT/PE (32.6%). The filter is designed to bioconvert at 60 days after implantation. At the time of bioconversion, the device’s nitinol arms retract from the filtering position into the caval wall and the stable stent-like nitinol frame is endothelialized. The composite primary 6-month endpoint of clinical success was achieved in 97.4%, no other filter-related symptomatic complications occurred, also no filter tilting, migration, embolization, fracture, or caval perforation and no filter-related deaths through 2 years. The rate of new symptomatic PE was 0% (n = 126) through 1 year. During the second year of follow up, 2 cases of new PE occurred, but it was after the bioconversion of the filter and at a timing that doesn’t imply the release of an entrapped thrombus. During the 24 months of follow-up, the bioconversion was successful to 96.5% (82/85) of patients and there was no evidence of late-stage IVC obstruction or thrombosis.41 The availability and use of a bioconvertible filter constitutes a step forward. Although short-term outcomes are promising, further investigation is needed regarding any effect of the long-term presence of the bioconverted and endothelialized Sentry device.
Conclusion
It is widely acceptable among physicians that AC therapy is well established as the treatment of choice for VTE. IVCF have an important adjunctive role to prevent a potentially fatal PE, particularly when AC is contraindicated or has failed. Which IVCF to use, when to use them, for how long they should remain in place, and which is the most effective removal technique remains a highly complex process with many variables to consider. Decision making should be based on a thorough patient selection, balancing costs and benefits. It is important to clarify the cases in which the placement of an IVFC to a patient who already receives AC therapy is beneficial or constitutes a risk factor, due to the potential complications. Patients’ unique characteristics will aid to determine on a permanent or a retrievable filter placement. The majority of eligible patients should be considered for a retrievable filter but they should be rigorously followed up for removal as soon as they are not needed anymore to prevent long term complications. While most frequently IVCFs can be easily removed, advanced retrieval techniques may sometimes be necessary. These should be attempted in the hands of experienced physicians to minimize the risk of retrieval related complications and permit retrieval regardless of their implantation time. Further research is mandatory, to support the current evidence guidelines and optimize filter utilization in the future.
Financial Disclosure:
None reported
Declaration of Conflict of interests:
The authors declare no potential conflicts of interest with respect to the research, authorship, and/or publication of this article
References
- Bikdeli B, Chatterjee S, Desai NR, Kirtane AJ, Desai MM, Bracken MB, et al. Inferior Vena Cava Filters to Prevent Pulmonary Embolism: Systematic Review and Meta-Analysis. J Am Coll Cardiol 2017;70:1587-1597.
- Naddaf A, Avgerinos ED, Chaer RA. Inferior vena cava filters: An update. Ital J Vasc Endovasc Surg 2014;21:17-23.
- Turner TE, Saeed MJ, Novak E, Brown DL. Association of Inferior Vena Cava Filter Placement for Venous Thromboembolic Disease and a Contraindication to Anticoagulation With 30-Day Mortality. JAMA Netw Open 2018;1:e180452.
- Jaff MR, McMurtry MS, Archer SL, Cushman M, Goldenberg N, Goldhaber SZ, et al; American Heart Association Council on Cardiopulmonary, Critical Care, Perioperative and Resuscitation; American Heart Association Council on Peripheral Vascular Disease; American Heart Association Council on Arteriosclerosis, Thrombosis and Vascular Biology. Management of massive and submassive pulmonary embolism, iliofemoral deep vein thrombosis, and chronic thromboembolic pulmonary hypertension: a scientific statement from the American Heart Association. Circulation 2011;123:1788-830. doi: 10.1161/CIR.0b013e318214914f. Erratum in: Circulation 2012;126:e104. Erratum in: Circulation 2012;125:e495.
- Kaufman JA, Kinney TB, Streiff MB, Sing RF, Proctor MC, Becker D, et al. Guidelines for the use of retrievable and convertible vena cava filters: report from the Society of Interventional Radiology multidisciplinary consensus conference. J Vasc Interv Radiol 2006;17:449-59. Erratum in: J Vasc Interv Radiol 2017;28:1338.
- Caplin DM, Nikolic B, Kalva SP, Ganguli S, Saad WE, Zuckerman DA. Quality improvement guidelines for the performance of inferior vena cava filter placement for the prevention of pulmonary embolism. J Vasc Interv Radiol 2011;22:1499-1506.
- Expert Panel on Interventional Radiology:; Minocha J, Smith AM, Kapoor BS, Fidelman N, Cain TR, Caplin DM, et al. ACR Appropriateness Criteria® Radiologic Management of Venous Thromboembolism-Inferior Vena Cava Filters. J Am Coll Radiol 2019;16(5S):S214-S226.
- Kaufman JA, Barnes GD, Chaer RA, Cuschieri J, Eberhardt RT, Johnson MS, et al. Society of Interventional Radiology Clinical Practice Guideline for Inferior Vena Cava Filters in the Treatment of Patients with Venous Thromboembolic Disease: Developed in collaboration with the American College of Cardiology, American College of Chest Physicians, American College of Surgeons Committee on Trauma, American Heart Association, Society for Vascular Surgery, and Society for Vascular Medicine. J Vasc Interv Radiol 2020;31:1529-1544.
- Johnson MS, Spies JB, Scott KT, Kato BS, Mu X, Rectenwald JE, et al. Predicting the Safety and Effectiveness of Inferior Vena Cava Filters (PRESERVE): Outcomes at 12 months. J Vasc Surg Venous Lymphat Disord 2023;11:573-585.e6.
- PREPIC Study Group. Eight-year follow-up of patients with permanent vena cava filters in the prevention of pulmonary embolism: the PREPIC (Prevention du Risque d’ Embolie Pulmonaire par Interruption Cave) randomized study. Circulation 2005;112:416-422.
- Mismetti P, Laporte S, Pellerin O, Ennezat PV, Couturaud F, Elias A, et al. Effect of a retrievable inferior vena cava filter plus anticoagulation vs anticoagulation alone on risk of recurrent pulmonary embolism: a randomized clinical trial. JAMA. 2015;313:1627-1635.
- Kakkos SK, Gohel M, Baekgaard N, Bauersachs R, Bellmunt-Montoya S, Black SA, et al. Editor’s Choice – European Society for Vascular Surgery (ESVS) 2021 Clinical Practice Guidelines on the Management of Venous Thrombosis. Eur J Vasc Endovasc Surg 2021;61:9-82.
- Sharifi M, Bay C, Skrocki L, Lawson D, Mazdeh S. Role of IVC filters in endovenous therapy for deep venous thrombosis: the FILTER-PEVI (filter implantation to lower thromboembolic risk in percutaneous endovenous intervention) trial. Cardiovasc Intervent Radiol 2012;35:1408-1413.
- Avgerinos ED, Hager ES, Jeyabalan G, Marone L, Makaroun MS, Chaer RA. Inferior vena cava filter placement during thrombolysis for acute iliofemoral deep venous thrombosis. J Vasc Surg Venous Lymphat Disord 2014;2:274-281.
- Kölbel T, Alhadad A, Acosta S, Lindh M, Ivancev K, Gottsäter A. Thrombus embolization into IVC filters during catheter-directed thrombolysis for proximal deep venous thrombosis. J Endovasc Ther 2008;15:605-613.
- Malinoski D, Ewing T, Patel MS, Jafari F, Sloane B, Nguyen B, et al. Risk factors for venous thromboembolism in critically ill trauma patients who cannot receive chemical prophylaxis. Injury 2013;44:80-85.
- Ho KM, Patel P, Chamberlain J, Nasim S, Rogers FB. Long-term outcomes after using retrievable vena cava filters in major trauma patients with contraindications to prophylactic anticoagulation. Eur J Trauma Emerg Surg 2023;49:335-341.
- Elkbuli A, Ehrhardt JD, Kinslow K, McKenney M. Timing of Prophylactic Inferior Vena Cava Filter Placement and Trauma Outcomes : Does Early Placement Matter? Am Surg 2020;86:1741-1747.
- Ghatan CE, Ryu RK. Permanent versus Retrievable Inferior Vena Cava Filters: Rethinking the “One-Filter-for-All” Approach to Mechanical Thromboembolic Prophylaxis. Semin Intervent Radiol 2016;33:75-78.
- Brothers TE, Todoran TM. Permanent inferior vena cava filters offer greater expected patient utility at lower predicted cost. J Vasc Surg Venous Lymphat Disord 2020;8:583-592.e5.
- Desai TR, Morcos OC, Lind BB, Schindler N, Caprini JA, Hahn D, et al. Complications of indwelling retrievable versus permanent inferior vena cava filters.J Vasc Surg Venous Lymphat Disord 2014;2:166-73.
- Eifler AC, Lewandowski RJ, Gupta R, Karp J, Salem R, Lee J, et al. Optional or permanent: clinical factors that optimize inferior vena cava filter utilization. J Vasc Interv Radiol 2013;24:35-40.
- Al-Hakim R, Kee ST, Olinger K, Lee EW, Moriarty JM, McWilliams JP. Inferior vena cava filter retrieval: effectiveness and complications of routine and advanced techniques. J Vasc Interv Radiol 2014;25:933-940.
- Deso SE, Idakoji IA, Kuo WT. Evidence-Based Evaluation of Inferior Vena Cava Filter Complications Based on Filter Type. Semin Intervent Radiol 2016;33:93-100.
- Desai KR, Pandhi MB, Seedial SM, Errea MF, Salem R, Ryu RK, et al. Retrievable IVC Filters: Comprehensive Review of Device-related Complications and Advanced Retrieval Techniques. Radiographics 2017;37:1236-1245.
- Avgerinos ED, Bath J, Stevens J, McDaniel B, Marone L, Dillavou E, et al. Technical and patient-related characteristics associated with challenging retrieval of inferior vena cava filters. Eur J Vasc Endovasc Surg 2013;46:353-359.
- Desai KR, Laws JL, Salem R, Mouli SK, Errea MF, Karp JK, et al. Defining Prolonged Dwell Time: When Are Advanced Inferior Vena Cava Filter Retrieval Techniques Necessary? An Analysis in 762 Procedures. Circ Cardiovasc Interv 2017;10:e003957.
- Desai KR, Lewandowski RJ, Salem R, Mouli SK, Karp JK, Laws JL, et al. Retrieval of Inferior Vena Cava Filters With Prolonged Dwell Time: A Single-Center Experience in 648 Retrieval Procedures. JAMA Intern Med 2015;175:1572-1574.
- Brahmandam A, Skrip L, Mojibian H, Aruny J, Sumpio B, Dardik A, et al. Costs and complications of endovascular inferior vena cava filter retrieval. J Vasc Surg Venous Lymphat Disord 2019;7:653-659.e1.
- K. Desai, R. Ryu, R. Lewandowski. Current IVC Filter Retrieval Techniques A problem-solving approach to retrieving embedded inferior vena cava filters. Endovasc Today 2017;16:65-69.
- Al-Hakim R, McWilliams JP, Derry W, Kee ST. The hangman technique: a modified loop snare technique for the retrieval of inferior vena cava filters with embedded hooks. J Vasc Interv Radiol 2015;26:107-110.
- Moriarty HK, Marshall E, Clements W. A 7-year retrospective review of the technical success of the “low-profile” hangman technique for complicated inferior vena cava (IVC) filter retrievals. Diagn Interv Radiol 2020;26:118-123.
- Tavri S, Patel IJ, Kavali P, Irani Z, Ganguli S, Walker TG. Endobronchial forceps-assisted complex retrieval of inferior vena cava filters. J Vasc Surg Venous Lymphat Disord 2019;7:413-419.
- Stavropoulos SW, Ge BH, Mondschein JI, Shlansky-Goldberg RD, Sudheendra D, Trerotola SO. Retrieval of Tip-embedded Inferior Vena Cava Filters by Using the Endobronchial Forceps Technique: Experience at a Single Institution. Radiology 2015;275:900-907.
- Chick JF, Stavropoulos SW, Shin BJ, Shlansky-Goldberg RD, Mondschein JI, Sudheendra D, et al. A 16-F Sheath with Endobronchial Forceps Improves Reported Retrieval Success of Long-Dwelling “Closed Cell” Inferior Vena Cava Filter Designs. J Vasc Interv Radiol 2016;27:1027-1033.
- Chen JX, Montgomery J, McLennan G, Stavropoulos SW. Endobronchial Forceps-Assisted and Excimer Laser-Assisted Inferior Vena Cava Filter Removal: The Data, Where We Are, and How It Is Done.Tech Vasc Interv Radiol 2018;21:85-91.
- Kuo WT, Doshi AA, Ponting JM, Rosenberg JK, Liang T, Hofmann LV. Laser-Assisted Removal of Embedded Vena Cava Filters: A First-In-Human Escalation Trial in 500 Patients Refractory to High-Force Retrieval. J Am Heart Assoc 2020;9:e017916.
- Desai KR, Xiao N, Salem R, Karp JK, Ryu RK, Lewandowski RJ. Excimer Laser Sheath-Assisted Retrieval of “Closed-Cell” Design Inferior Vena Cava Filters. J Am Heart Assoc 2020;9:e017240.
- Eggers MD, Reitman CA. In vitro analysis of polymer candidates for the development of absorbable vascular filters. J Vasc Interv Radiol 2012;23:1023-1030.
- Thors A, Muck P. Resorbable inferior vena cava filters: trial in an in-vivo porcine model. J Vasc Interv Radiol 2011;22:330-335.
- Dake MD, Murphy TP, Krämer AH, Darcy MD, Sewall LE, Curi MA, et al. Final Two-Year Outcomes for the Sentry Bioconvertible Inferior Vena Cava Filter in Patients Requiring Temporary Protection from Pulmonary Embolism. J Vasc Interv Radiol 2020;31:221-230.e3.